The Fourth of July is around the corner, but the United States isn’t quite ready to declare its independence from the coronavirus. So what’s the safest way for Americans to carry out their holiday plans?
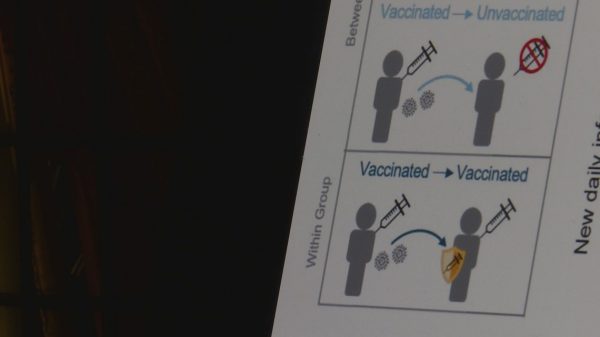
That primarily depends on your vaccination status. As health officials sound the alarm over the new, highly transmissible delta variant, people who have completed their COVID-19 vaccine series are well-protected from the disease. Fully vaccinated people can resume their pre-pandemic social lives, per guidance from the Centers for Disease Control and Prevention, including gathering inside or outside with friends and family.
But those who aren’t vaccinated or who are less than two weeks out from their final dose are at risk, and partially vaccinated people should still behave as if they’re unvaccinated.
That means taking precautions to avoid infection, like wearing a mask inside and staying outdoors when socializing with people who aren’t in their immediate households.
“[For] unvaccinated people, nothing has really changed since last Fourth of July,” said Dr. Leana Wen, an emergency physician and public health professor at George Washington University.
But it isn’t always as straightforward as making choices based on your own vaccination status. Maybe you’ve got kids under the age of 12 who aren’t yet eligible for a COVID-19 shot, or medical conditions that mean your doctor has recommended a more cautious approach to your social life.
Choosing COVID-safe July 4th activities requires an assessment of both vaccine science and your personal risk tolerance. Here are some tips you can use to make those calls for yourself and your family.
How to throw a pandemic-safe gathering
First, the good news: Spending time outside without masks is generally a safe option for everyone. However, when it comes to parties, barbecues and other Fourth of July festivities, precautions may need to be taken if you’re going to be in close quarters with other people.
Here, again, it mostly comes down to vaccination: Those who are fully vaccinated can celebrate like they would in any other year. (Though maybe hold off on the fireworks, for other reasons.)
If you’re not fully vaccinated and plan to spend time with other unvaccinated or partially vaccinated people, the CDC recommends masking up outside — including at both large and small gatherings and at restaurants. This is particularly important if you’re in a community where the coronavirus transmission rate is high.
Socializing indoors is the least safe option for unvaccinated people, and should be avoided or done with proper masking.
“I’m not concerned about outdoor transmission,” Wen said, noting that she regularly gathers with other families outside, where their young, unvaccinated children can safely play and even eat together. “I’m worried about what occurs indoors.”
Even for the fully vaccinated, the risk of spreading COVID-19 to others or becoming ill with the disease themselves is not nonexistent, Wen said. That’s because although COVID-19 shots offer high levels of protection against infection, and particularly against severe disease, no vaccine is completely effective.
It’s highly unlikely that fully vaccinated people will be hospitalized or die as a result of the disease. But those who want to take additional precautions, like people with some medical conditions, have options.
Immunocompromised people, for example, can take precautions like masking up in any public place where they can’t be sure about another person’s vaccination status. But spending time outside, especially with other fully vaccinated people, is a fairly safe bet.
WATCH: Highly contagious delta variant on path to become dominant strain in the U.S.
“As long as there’s some air flow, you’re going to be OK outdoors [unmasked,] even if you are immunosuppressed. But I would still wear a mask at indoor gatherings where you’re not sure that everyone around you is vaccinated,” Ranney said.
If that’s you, spending time only among fully vaccinated people is “the safest thing to do,” Wen said, who also urged anyone with medical concerns to “talk to their doctor about their individual circumstances.”
Ranney noted that fully vaccinated grandparents can generally see their unvaccinated grandchildren inside or outside safely, particularly if everyone who’s eligible within the family is fully vaccinated. But she recommends masks for everyone involved when spending time inside with someone who is taking immunosuppressants, or when gathering indoors with unvaccinated children from multiple households.
Regardless of your vaccination status, if you have symptoms associated with COVID-19, cancel your Independence Day plans, get tested and quarantine.
What to do if someone tests positive
Let’s say you go to a picnic and, several days later, discover that another attendee tested positive.
The CDC says that if you’re vaccinated, you don’t need to get tested unless you develop symptoms. But Wen also recommends using some nuance and critical thinking when it comes to making that choice, especially if a closer contact ends up testing positive.
“If you saw somebody briefly for a few minutes at a party and then that person tested positive, that’s very different from if you live at home with someone and your partner has now tested positive,” Wen said.
People who are unvaccinated and discover they have been exposed should isolate themselves from other people and get tested between five to 10 days from last contact with that person. That’s because it takes time for enough virus to generate in the body to result in a positive test if you have been infected. If you develop symptoms at any point after being exposed, however, you should get tested immediately.
“Is it ever wrong to get tested? Is it ever wrong to wear a mask? No, it’s not a wrong thing to do,” Ranney said. “It’s a cautious thing to do.”
Delta variant yet another reason to get vaccinated
So far, the emergence of the delta variant has not prompted the CDC to change any of its guidance for fully vaccinated people. Health officials are primarily concerned about how this variant could impact unvaccinated and partially vaccinated individuals.
“The delta variant is certainly concerning, but so is COVID in general,” Ranney said. “It’s not a brand new disease, it’s just a little bit more transmissible. It’s easier to catch it. But the same basic precautions work for delta.”
Wen noted that this variant is about 60 percent more transmissible than the alpha variant that drove surges in multiple countries during the winter months. That means that unvaccinated and partially vaccinated people are now even more vulnerable to COVID-19 infection if exposed.
Communities with low vaccination rates, particularly in some parts of the South and West, are at the highest risk for transmission of this variant.
WATCH: Dr. Fauci on delta variant, booster shots and masks for the vaccinated
Dr. Anthony Fauci told the PBS NewsHour on Tuesday that the delta variant is “a clarion call” for unvaccinated people in any part of the country to get their COVID-19 shot as soon as possible to protect themselves and others.
“You don’t want to see two Americas, one that’s protected very nicely because the vaccines work, and then certain pockets of the country where you can have these mini-surges which could really be very disconcerting and dangerous,” Fauci said.
The World Health Organization recently urged people to wear masks to deter the spread of the delta variant. Fauci noted that the WHO is an international organization that serves the global population, around 10 percent of which is vaccinated, and that some COVID-19 vaccines distributed in other countries offer far less protection than the ones used in the U.S.
As one of the richest countries in the world (albeit, one with one of the worst wealth disparities), Americans are comparatively better off due to the nation’s resources and robust vaccine rollout — more than 50 percent of the eligible population is now fully vaccinated — and low disease transmission in highly vaccinated communities.
Disparities also persist, even in cities where vaccinations are high, among residents by race and ethnicity. In many places, Black and Latino residents are getting vaccinated at lower rates compared to other groups, and also are more likely to be hospitalized or die as a result of COVID-19. If current vaccination trends continue, the disease could continue to disproportionately impact those who are already most vulnerable to it.
Overall, Americans are growing more optimistic about the ways their lives are returning to normal, according to a PBS NewsHour/NPR/Marist poll released Thursday. But even with a significant portion of the population vaccinated, half of U.S. adults say they still fear another surge could come. No matter how you’re planning to enjoy the summer, health officials agree: the pandemic is not over and it’s OK to take a raincheck this year.